Hey ladies! Did you know that apparently you’re supposed to prioritize your future children over yourself when it comes to receiving (possibly life-saving) healthcare? Even if those children don’t currently (or will never) exist?
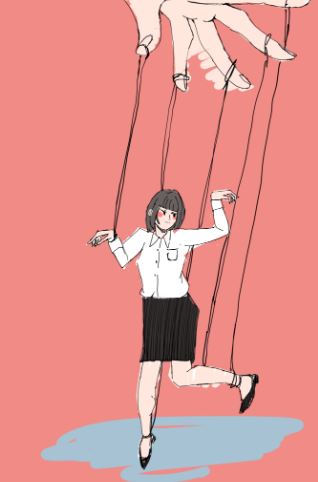
Most women are well aware that society expects them to get pregnant at some point in their lives. (I realize that not everyone who identifies as a woman is capable of biological pregnancy, but I use the term nevertheless since this article discusses society’s outdated views of womanhood.) But in addition to being paternalistic and condescending, this perception has dangerous implications for pregnant women and non-pregnant women alike. A major factor is the concept of fetal protection ethics, a principle that essentially states that fetuses, even if they don’t exist yet, should be valued equally to their mothers. This affects virtually every aspect of women’s healthcare due to regulations on scientific trials and, subsequently, the availability of gender-specific medical data.
As late as the 90s, the Food and Drug Administration (FDA), National Institutes of Health (NIH), and other international and national research regulators automatically excluded women with “childbearing potential” from early-phase drug trials (regardless of whether or not these drugs were even meant to affect pregnancy in the first place). One government official succinctly pointed out that the FDA’s rules instructed that scientists should assume that “all women are pregnant unless proven otherwise”. The reasoning was that since “women are born with all the eggs they will ever produce, they should be excluded from drug trials in case the drug proves toxic and impedes their ability to reproduce in the future.” As a result, on average, women make up just 22% of participants in phase 1 trials, as of 2020.
That’s a lot of missing data! Not only were these policies inherently unjust since they treated women like walking incubators, but they have also led to a large gender gap where scientists have far more information about men’s experiences. This has extensive healthcare-related implications. For example, women 一 especially those aged 18-34 (ages that happen to make up most of a woman’s potential childbearing years) 一 have higher adverse drug reactions than men. A government audit of 10 drugs withdrawn from the market between 1997 and 2000 found that 80% of adverse drug reactions predominantly affect women. Women also wait longer on average to be diagnosed and to receive pain relief, mainly since most medical data has been collected from men and generalized to women.
Despite major strides in the inclusion of women in scientific trials, society’s treatment of all women as mothers-in-waiting remains a significant issue. As recently as 2016, the Centers for Disease Control and Prevention (CDC) released a statement urging women in their childbearing years to avoid consuming alcohol if they were not currently on birth control 一 lest those women’s choices harm future pregnancies. (For what it’s worth, pre-pregnancy drinking has never been proven to cause birth defects, but this is certainly not the first time medical recommendations have relied on stereotypes and condescension rather than evidence.) Even more recently, the Supreme Court Dobbs v. Jackson Women’s Health Organization decision, which overruled the constitutional right to abortion, has further perpetuated a perception of womanhood and motherhood considered intertwined 一 and women face the consequences of this perception. For example, pregnant women have historically received more healthcare opportunities than non-pregnant women. Prior to the Affordable Care Act, many states only provided comprehensive health coverage to low-income women if they were pregnant.
Additionally, even though conception is a joint venture between men and women, most (if not all) of the responsibility for pre-pregnancy care is placed on women. An alarmingly high number of healthcare providers follow an “every woman, every time” approach, in which every encounter they have with a woman is viewed as an opportunity to increase her health for future pregnancies. A major reproductive health expert has even suggested that “every routine primary or specialty care visit and family-planning visit (especially those that include a negative pregnancy test) is an opportunity to provide preconception care for health promotion, disease prevention, and reduction of prenatal and neonatal complications.” Despite the evidence for the benefits of this approach being weak at best, this approach has inspired major public health programs in various states, including California, Florida, and North Carolina. In a move that surprises absolutely nobody, the state of Texas has long deemed that “provided it is subsequently born alive, even an unborn fetus is a “patient” to whom a doctor treating the mother owes a duty.” (Of course, there’s no way to know if an unborn fetus will be born alive or not, especially considering that miscarriages are far more common than people realize and cannot be prevented.)
This sort of medical surveillance of women continues. Since the Dobbs decision was released, many pharmacies and physicians have been forced to deny or delay patients’ access to various medications, such as methotrexate, which is used to treat an array of cancers and autoimmune diseases. In one case, a pharmacist initially refused to dispense methotrexate to an 8-year-old girl in Texas, writing that “females of possible childbearing potential have to have a diagnosis on hard copy with state abortion laws.” That child is not the first patient for whom pregnancy has been taken into consideration before receiving life-saving healthcare, even though ultimately it shouldn’t matter 一 pregnant women also deserve to make their own healthcare decisions, and potential risk to the fetus is ethically irrelevant. Instead of promoting gender equality, both healthcare providers and legislators are stagnating advances in women’s health, if not outright making it worse. It’s no wonder that the U.S. ranks last for women’s healthcare among wealthy developed countries.
Enough is enough. Here’s an idea for doctors: let’s treat women the same way we treat men (i.e., as human beings with potential beyond being future baby-makers). This means that future pregnancies should be treated as irrelevant for most women, and pregnant women should not be automatically excluded from medical trials (yes, this continues to occur and will most likely remain standard practice for the foreseeable future). While obviously women who express interest should receive information about the potential risk to potential fetuses, it is paternalistic to assume that every woman wants to be a mother — and it is akin to medical malpractice to let half of the world’s population continue to receive inadequate healthcare.

Comments